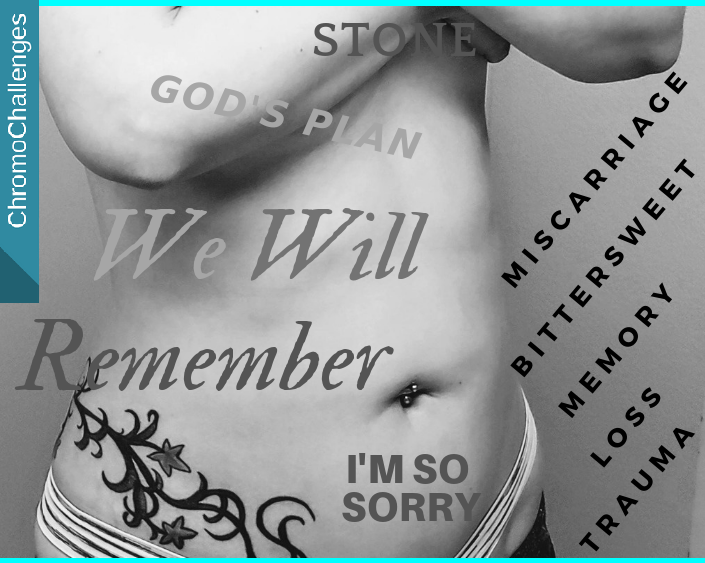
Aubby’s Trisomy 18 Birth Story

To tell my daughter’s birth story is not an exercise in having had a “successful birth experience” in the Trisomy 18 world, but having had a successful GROWING experience.
Even three years later, my body still tenses when I recall my pregnancy with her. I remember extreme resentment towards the medical professionals that discouraged hope or any iota of joy I tried to feel. It was a deep depression that stayed with me… through later pregnancies I lost, which I felt was maybe in part due to having had hope killed from me in that first pregnancy.
I still recall my pregnancy with my daughter with anger that, without any official prenatal diagnosis as I listened to my gut and opted against testing, that it was still suggested that I abort when ultrasound showed she had a blockage in her bowel. She also had a 2-vessel cord and growth rate in the 28th to 33rd percentile all pregnancy, but I don’t see how that warranted that judgment lock, stock, and barrel without an official diagnosis. It was suspected she might have cystic fibrosis, but why tell me to abort on a suspicion? Because I listened to my own feelings? Or was she just a small baby because of having a 2-vessel cord and just happened to have an issue with bowel development?
More often than not for such families, insurance and hospitals refuse to intervene in the immediate medical needs of a baby born with Trisomy 18. Or even a variant, partial T18, like my girl. My gut feeling was right not to get prenatal testing, for she would’ve been treated entirely “incompatible with life”, which she’s proven entirely false, and getting her surgeries done would have been far more difficult, if not impossible. Sure, my life would have been less complicated, but it wouldn’t have been happier without her.
But you have to ask: What does “incompatible with life”… mean? The base implication is whether congenital health impacts involved outweigh doing anything about them. As in, Is it ethical to perform surgery on a newborn?
In the case of my kiddo, and so many others whose fates are not-so-obviously sealed, it should be ethical. There’s enough advancement medically for there to be great quality of life in individuals who have Down Syndrome. Being the next-most prevalent chromosomal condition in newborns, how is T18, therefore, different? Except doctors are still taught 30-year-old information when heart intervention is the top need for T18 (and T13) children in order to give them a fair chance at living and to come home to their families without the long shadow of an expiration date.
And then there’s the dismissal of children and adults who have disabilities. Is it ethical to intervene at all, as if people who have disabilities don’t feel joy, or appreciate the lives they lead, or have families who love and care for them? The ethical question among health professionals becomes, Are they too great a burden?
And so on.
Compatibility with life, really, becomes default, the refusal to die.
As it was, in the days after her birth, and in the first hours that I first got to see her after two days apart — immediately after birth until I was allowed to see her, since I had a minor fever from a light hemorrhage from delivering — I heard doctors point out ways she was “abnormal”. That’s the word they used over and over. I quietly stood in the room staring, wondering and in wonder, at her beauty while they talked and said that word like I wasn’t even there.
I feel indignant to this day that I’ve had to fight since Day 2 when I finally met her to somehow prove that she’s worth fighting for against others’ prejudices. Somehow they see a diagnosis wearing a face, and I see my growing child who’s been far braver than they ever were. And they suggest I give up when she’s done so much.
Every emotional trauma, mental anguish, and physical deprivation as I held vigil at her bedside for 6 of the 7 weeks she was in NICU care that was split between two different hospitals…
The deep loneliness being apart from my husband who had to work through all this, his own pain at being away from us during that time… (But how could she be safe without at least one of us to watch over her?…)
She was, has been, and will always be worth it.
Every bit of backbone earned as we were told so many times that she’s not worth the investment of energy, that she’ll never do this or that, that she’s incapable of that or this…
Because we appreciated and nurtured her worth, our efforts brought her through the mad darkness we lived through her first three years of life.
Surgeries
I can assure every doctor who’s ever seen my daughter that the surgery for the bowel blockage was worth it. The blockage could’ve ruptured during my pregnancy with her, but didn’t. And that surgery was — understatement — a big event for a four-day-old. But it saved her.
That surgery wasn’t performed at the hospital that she was delivered at because her surgeon had a family emergency. Due to his family emergency, it was required she be transferred to a bigger hospital two hours away. And as true as that might’ve been that time, he had regular emergencies and vacations during most other occasions she ever needed care. In all, I’m still glad the transfer hospital took such good care of her.
The week after that bowel surgery, they still took good care of her through an infection which nearly sent her into complete respiratory, heart, and kidney failure. But, somehow, in spite of the doctors’ fears and through my stark agony as they reintubated her, she stayed alive.
She stayed alive through PDA heart repair by catheter. She got through that there with what they said was a routine hiccup when something inside was bumped and she had AFib (irregular heartbeat) for a moment… Following a hard discussion with her doctor whether cath or an open surgery through her side would be best. I like solid permanent fixes, but the cath was correct. She received the cath. It went well. It was completely worth it.
It was her second-and-a-half week of life, after the cath began to take effect, when I saw her skin pink up for the first time from that awful oxygen-deprived pallor.
Then she was finally able to handle real sustenance for the first time, and the IV was replaced by an NG tube that went in her nose to her stomach for breastmilk I’d faithfully pumped since her birth.
Her breathing improved.
Her enlarged heart stopped working so hard and returned to a more normal size.
She finally evinced physical energy instead of the floppiness of her early days. She was able to wake more.
Our little fighter began to live.
Microarray Says? Partial Trisomy 18
She was three weeks old when the transfer hospital’s genetic counselor gently informed me that our microarray results were back and that she had a chromosomal condition with no knowable outcome. She said our daughter may be unaffected, or may be severely affected. That our daughter may not live, or would live much longer. But that while it wasn’t my fault, I had a genetic arrangement, a Balanced Translocation, that predisposed her to it.
Still, she stayed alive. Those days at the transfer hospital were graced, for they treated her like a person even to using her name.
But when we were transferred back to the hospital she was born in, she made it through more substandard treatment like after she was delivered. Back at her original hospital, she was underfed, I was not told the truth about what food she was receiving, my husband and I were cornered by a set of three genetic counselors who told us she would absolutely die by eight weeks old… And so on.
I wish I could go back and change how that went. We should have reported them, not had to defend ourselves at every turn. But They were not our immediate problem. Proving Aubby’s worth and her will to fight was. So she received a feeding tube at six weeks old, and we were able to go home when she was about seven weeks old.
I wish I could say our return home was when things got better. It wasn’t. Starting out, neither my husband or I slept those first three weeks.
I couldn’t sleep because every irregular breath she had, and figuring out she’s the kind of person who sleeps with her eyes open, kept making my stomach feel punched. When I saw her with her eyes open during this or that spate of sleep apnea I kept thinking This Is It, that the counselors were right that she was about to die. I desperately didn’t want them to be right.
My husband didn’t sleep because my sleep was so fitful, and because we had to keep her fed. We were up every single 90 minutes to make sure her feeding pump was run, that I kept up pumping to supply her food, and that she wasn’t aspirating anything. “Exhausting” wasn’t near the right word for it. And it turned out that her most active time to be awake was 2:00 a.m. to approximately 5:00 a.m., a habit that’s hung on past turning age three.
Corn Allergy
While in the hospital, she was called “failure to thrive”. After we were home, I discovered a far different trend.
I started upping her feed amount by 15 ml a week, average. Because she wasn’t satisfied. I finally found out what “satisfied” actually looked like for her. And realized that the amount she was receiving in hospital care was chronically about 1 oz per feed less than was correct for her because they refused to move her breastmilk schedule from the formula amount and frequency to what was right for breastmilk. So it wasn’t until she was three months old, out of hospital for a month, that she started putting on any weight.
Her doctors didn’t think she was gaining fast enough. We were told to fortify, it was insisted on. So between three and five months old we included formula in her breastmilk feeds. Except then, she had severe gastrointestinal pain from 10 minutes into a feed until it had digested at the 2-hour mark. Severe pain, cramping, simultaneous diarrhea and constipation, red bumps on her face, reflux, bloating, you name it.
She experienced the same through five different formulas, from Neocate to soy to hypoallergenic. I finally refused to fortify — what’s the point if she’s just going to vomit away her progress? She started gaining weight again on my breastmilk. Nevermind we were told she was incapable of using a bottle or nursing, she took to nursing too. I pumped 25 oz each day in addition to the approximate 10 oz she took on her own each day. And so it went until she was 10 months old and looked like a little Michelin baby.
It was when she was 10 months old that we discovered her first real allergy. I introduced corn as a new jar baby food. She threw up all night long. At first, I thought she’d had a bad bag of breastmilk because we had her stash in a cooler since we were at a festival. But in trying the jar food again the next day, she threw up again. It was the corn! And guess what main ingredient is in powdered formulas? Corn. Corn syrup, corn starch. That’s why she couldn’t tolerate the formulas when it was insisted we fortify my breastmilk.
More concerning was that, at discharge point from hospital, I’d found out she was being supplemented with formula even though I’d asked on three occasions while there whether she was receiving other food. The original NICU that we were transferred back to had told me all times I’d asked that she was only receiving breastmilk. In retrospect, I now believe my wishes for her care were ignored “for her own good” because only “crunchy moms who don’t vaccinate their kids” swear by exclusive breastmilk for babies. If I’d just been told the truth, at least I could have narrowed down the issue faster.
Corrections and Milestones
The day she turned eight months old she said her first word: a long, soft, drawn-out “Hiiii…” It was so sweet. That was the first time she proved she has more going on in her mind than she ordinarily let others in on. She’s gone on to say a couple handfuls of words and a couple phrases between then and 3 years old including Hey, Hello, Ow, Daddy, Mama, I love you, and repeated “of the tiger” after hearing the song “Eye of the Tiger”.
Our next hurdle was scoliosis. From age six months to turning a year old, due to global physical delays she developed a flexible 17-degree curve in her spine. The Child Development Clinic, a clinic part of the hospital network she was born in, said she’d need surgery “soon”. She was a year old! After some research, and after my husband serendipitously met a chiropractor at the Farmer’s Market, we took Aubby to see the chiropractor. He was able to reduce the scoliosis she had from 17 degrees to 0 degrees. In three weeks.
Also supporting improvement of scoliosis, and hip dysplasia from her leg being up next to her head before she was born, I began to babywear her in an Infantino Mei Tei carrier.
From 7 to 10 months, we started working on practicing eating jar foods by mouth. It took until 10 months before I figured out an approach that worked with her, and then she loved eating oral food so much! So much that at 13 months old she chose to self wean. No more nursing! I felt a bit blue when she self weaned; I’d intended to breastfeed her to 18 months old. But 13 months of nursing my impossible infant was its own triumph. Weaning went very smooth.
Because she weaned a bit earlier at 13 months old than anticipated we were able to switch her to a formula I had researched. As it turned out, a good nondairy, noncorn option was (AFFILIATE LINK) Similac Alimentum RTF (ready to feed) liquid formula (available at Walmart and other places). She stayed on Alimentum RTF until 15 months old when her weight plateaued and was then switched to Compleat Pediatric formula.
At 11 months old, she rolled over front to back AND back to front for the first time, and between 13 and 15 months she started to scoot herself across surfaces. This first showed itself when she scooted not forwards, but backwards and started wedging herself under furniture!
At about 15 months she underwent surgical correction for an umbilical hernia, and removal of a urachal cyst in the same procedure. That was the surgery that led to finding out about IV ultrasound teams in hospitals after she lost her IV in Recovery and had to heal only using Ibuprofen and Tylenol. I felt awful for her, she was in such pain, but also so proud that she had the experience to “hoss” through it. Strong girl.
And wouldn’t you know it? It took until she was 20 months old(!) before her first tooth cut in! The average I’d read in a SOFT guidebook about Trisomy 18/13 was at most 15 months, but in the nick of time before more hormonal reasons were going to be explored, her first tooth came in. Teething was its own special place. From 20 to 38 months of age, she teethed 2, 3, or 4 teeth at the same time. It regressed her oral eating skills, and there were terrible weeks she just screamed when she was awake for four days straight, day and night. All that time, the only fixes she responded to was Tylenol or being held and rocked. She hated cold things on her gums with a vengeance, and vibrating teethers didn’t even do the trick… The day that last molar came through was the best.
And Compleat Pediatric formula wasn’t the end of her food development. At 23 months and another weight plateau, we tried Nourish. Coming off Compleat Pediatric formula reduced her reflux and decreased the frequency of some stomach bleeds she was having. Nourish worked until she showed too much stomach gas (due to broccoli). At 24 months we were able to try Real Food Blends (RFB) instead, but then it turned out she had an allergy to grapeseed oil and a couple other things and could only tolerate one RFB option. At which point, a family member gifted me with some birthday money that I was able to spend on feeding supplies to move her to a fully blended whole food diet.
More Allergens
Her next big hurdle didn’t come for some time, not until she was a couple months shy of turning 3 years old. She started having intussusceptions (telescoping bowel) about once a week from October through December 2018.
I realized what some of my observations meant since she was hospitalized long enough to make them apparent. She was vomiting after coming home but not vomiting when away. We figured out she was severely pet allergic.
Removing her from an environment of pet allergens relieved a large part of her severe reflux and made it a more minor issue. To then, she hadn’t gained weight for 18 months. Then, she started gaining weight, had less drainage, and became a lot more sleep safe.
By then it was November and she’d had blood drawn and skin patch allergy testing. The results came back, in addition to confirming dairy and beef allergy, that she is moderate-severely allergic to fragrance mix II, too. That allowed my husband and I to switch her to an organic child shampoo, which brought relief back to her bath times.
She’d started out on an organic baby shampoo with no additives, but some of our home nurses started to use our adult shampoos no matter how often I told them to warn us if they noticed her shampoo running out. Aubby had no rashing or other indicators for allergy from those adult shampoos, except she panicked during baths of a sudden.
My best guess after reading about the effects of the fragrances she’s allergic to and effects of toxicity is that she must have felt a burning sensation during baths. I’m thankful for the allergy testing she had. Baths have become a joy for her again. She loves splashing.
Since she was still experiencing intussusceptions that I could just not find an answer for, the other matter was resolved on a prayer and a whim. In search of gastrointestinal affectors, we eventually tried including her on a gluten free diet like I was already having to follow since four months post partum.
The intussusceptions just… stopped. Finally. Earlier in October she’d had blood testing for celiac and was determined not to have it. I feel had she actually been scoped to check for it that it would have been confirmed for sure. But with the end of intussusceptions, she also stopped having what had become regular (for the past 18 months with no discernable explanation than “reflux?”) stomach bleeds, and a persistent constipation she had has become manageable.
After those two big changes, she improved so much! Far less vomiting. Better sleep. Better playful attitude, even.
We’ve just only had to adjust for further reflux issues.
More Milestones
She’s still largely nonverbal and doesn’t use sign language effectively but indicates yes or no with her attention/eyes, lifts her arms when she wants up or out of a chair, can scoot off of furniture or point herself down so she can slide to the floor when she wants down, and points at preferred foods at mealtimes or when making a choice. She helps put her shirts on by taking her arms out or in her sleeves. Sometimes she goes to an activity she wants, such as if she’s hungry earlier than a mealtime she’ll go to her high chair and wait, or sometimes she’ll go to her bed without prompting. She’s also started “checking on” my husband and I when she wants to make sure we’re where she can see us or are nearby such as when she isn’t up yet for the day, then wanders off to play.
Her next big development after teething began was pulling up and cruising, which she started at 24 and 26 months. We’ve been working with her and a reverse walker since then. Although she started with a larger walker that had a 30-pound weight on the back end, switching to the light model was far more encouraging for her since least-restraining equipment has always been her preference. At 42 -43 months she is still only cruising and using the reverse walker, but I have hope (no promises, but I am hopeful!) she will make the final leap to independent walking in the next year or two.
In March this year, she got glasses to counter severe astigmatism and coloboma in her left eye, and less-severe astigmatism in her right eye. It’s her first pair of Zoobugs, and I think she needs a different style of glasses to fit her face and ears better, so we’re being patient while she keeps taking them back off.
In Sum (For Now, as of the date of this post)
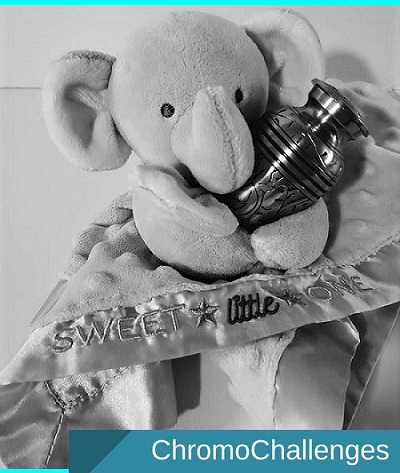
So many families I know are so sad about their babies growing up. After fighting so hard to make sure my girl could, I find it impossible to cry sad when she’s had another growth spurt. I’m always crying grateful she has. As I appreciate the new change, my way of missing her being small is to feel each moment as it fades into the next. Not missing her baby days like others do of their children is a strange place to be.
I know most of all I’ve written is medical. Milestones, and struggle, and measured steps, and progress. It can be disconcerting to remember that there’s a little girl under all that pressure, and not just a series of successes climbed.
Though, I feel that I remember there’s a little girl under all that pressure better than her doctors have done so far. I was the one who could see her so clearly in the NICU, could read her cues, knew her. As she merges into preschool and activities towards her development outside our home, I see more and more sparkle in her personality as we start to grow away from those terror years between 2015 and 2018.
That sparkle’s been a long time coming, after so much suffering… Like, until she got her glasses she was so sensitized about anything touching her face. Her time in NICU enduring oxygen tubes and NG tube changes had ingrained itself in her mind in the form of reflexes and, at times, unsettled sleep as she’s grown from her infant days. Things I hadn’t realized made such an impression until I saw her made the same faces she did when an oxygen tube blocked her from making sound. There are many small things like that I’ve noticed and recall when they first happened and I understand her whys all the more.
I love the little independent person she is. She’s sassy. And has her own jokes she makes, like when she licks our shoulder when she’s picked up, or biting a pantleg when she hops on one of mine or her Daddy’s feet to get a foot ride, or makes raspberry sounds instead of just using the potty when she asks to go to the toilet. She finds some things so funny, like if someone sneezes or clears their throat. She’s so curious about things and loves to study toys and scenery. She loves Ozzy Osbourne’s music, any music video featuring “The Prince Of Darkness”. And she loves books! She loves books and being read to, and has dragged out her Cuddle Bug book for me to read to her at least twice each time she sees it.
There’s no way for me to sum up any part of who she is. Except to say she’s a person who lives with a diagnosis — a real person and not a diagnosis who happens to have a face.
I wish doctors could see the incredible people that Trisomy kids become far more often than they think they can or know about.
I wish medical students were taught how strong Trisomy kiddos really are, and how it is that they grow beyond expectation. Even if it’s only for a day, or a week, or less than a year. It’s still time that matters. And maybe that time matters less to an ethics panel, but it matters to those families who face those panels. And it matters to those children who have the chance to see a “half birthday” or weekly/monthly celebrations of living, and those kiddos who make it to age one, and those kiddos who keep on keeping on.
It’s important to never give up. Never give up! There’s no giving up until the conclusion has come and gone. Because the impossible happens far too often to say that the end really is arrived.
After being sent home to “enjoy the time we had” (one of the tritest phrases I’ve ever heard), I lived my daughter’s first six months of life mourning her. Mourning her! Mourning that I couldn’t imprint every little finger and everything else and the sound of her cry and the shape of her eyes in my mind. If she had met the fate the hospital she was born in had envisioned, I would never have had the chance to forgive them their absence of compassion and wisdom… even if that did come, much later, when she almost succumbed to that first intussusception, as my husband and I still had to live in proximity of that hospital network, and I had to push back at their lack of care.
I wish medical staff focused not on limitation but on what’s possible. It’s not false promise to say that miracles happen – Trisomy families know miracles every day. Enough “miracles” that the label “incompatible with life” is known among Trisomy families as inaccurate if the care standard for children with Edward Syndrome were improved to ready intervention. Not all Trisomy families, no, and not a majority, but many more than many doctors might expect.
My daughter is a miracle, and is a beacon of my heart. I’m so grateful for the lessons she’s taught me and my husband as her parents and caretakers. She proves that the impossible is doable.





Very well done, Jessica. Aubby is such an amazingly strong child, and you are a brilliant mother. I truly believe you saved your daughter’s life, with your hawk-eye catches of her symptoms and comforts. Thank you for sharing your story!
<3
Holy #$%! I love this. Your wisdom and unwavering determination to stand up for your daughter in the face of rejection from American Healthcare is beyond words.
Redefine what is possible (or impossible) and give hope to back families dealing with T18 or other conditions!
Thank you! I do try my best. <3