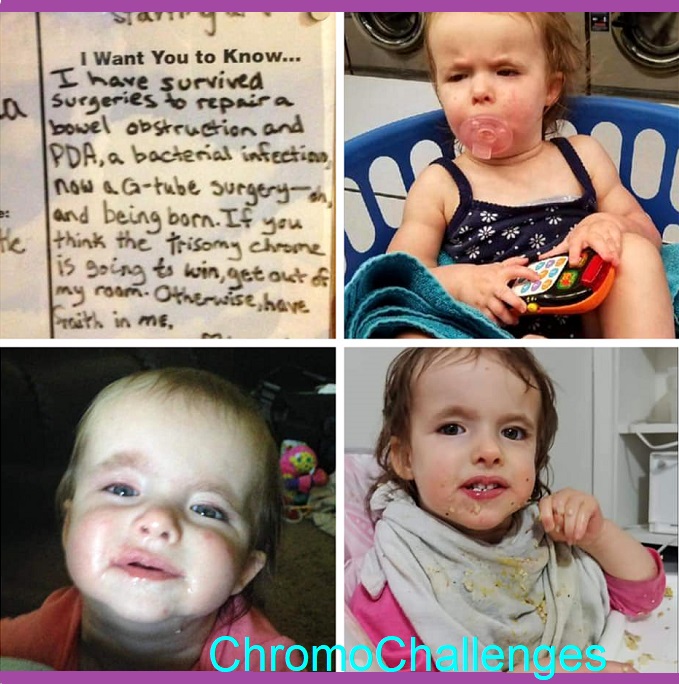
Trisomy Awareness Month
Trisomy 18 means there’s a third copy of the eighteenth chromosome, so Trisomy Awareness Month is March of each year, completing on the 18th of the month. The Trisomy community takes this time to remember our Warriors, living and angel.

DAY 1: Trisomy 18, Diagnosis Day, Pregnancy

Our Diagnosis Day wasn’t until 3 weeks after delivery. That was the day doctors stopped caring, until she was 8 months and still not dead and they had to begin to acknowledge her name during appointments. No more “x-months-old female”… but her Name in paperwork then.
My gut instinct had very strongly said not to do amnio, so I followed that feeling. In retrospect, as I didn’t find a good T18 support group until three months after diagnosis, I likely would have aborted because of what medical literature still says. I would never have gotten to know my girl. And had I had the amnio, she’d have been denied care and the initial surgeries needed right after birth.

Pregnancy was a little annoying because everyone said I was showing too small. I didn’t get bigger until later with polyhydramnios that started after the flu/dtap jab. I had super bad sciatic pain all pregnancy. Aubby, who then was dubbed ‘Wiggly’, was breech from Month 6 through two weeks before birth at 39+5. I was practically vegetarian, as meat smells were intolerable for me. I ate a lot of cucumbers.
DAY 2: Finding Fair Care

Aubby’s prenatal care was unfair for the sheer amount of stress impressed upon me by doctors, doctors telling me to abort without diagnostic testing results even on hand, and immediately after birth when her surgeon began a pattern of backing out of her appointments.
To complete her first surgery, the one she was known at Month 6 and forward of pregnancy to need, our family was transferred to a larger hospital. Transfer Hospital at least used her name, and they did right by her.

Then she was 3 weeks old when her chromosomal microarray came back. I was informed that I was infertile (but later had a chromosomally typical second child), and that her future was very uncertain. We were transferred back to our original hospital, where they proceeded to lie to me about some details about her care, bully me about not wasting my energy helping her, not submit SSI paperwork I’d been given to complete to even get home nursing resources (found that out a year later), and chronically underfeed her.
Then when we were discharged, I was given a stern talking to by the NICU head nurse about not asking for help because I was just a new mom. And that turned out that her feeding tube site was leaky, so acidy and burning… and I had to figure that out, by myself…
My husband and I were sent home under warning to “enjoy the time we had” and that she would go at any time. So I didn’t sleep, oh, for three weeks…
I’m no less angry at the entirety of it all, here five years later. But it is five years later. And they were all wrong.
DAY 3: Birth Story & Coming Home

As I’ve already written about our birth story, I’ll cover how it was coming home… After the NICU test for me to take care of Aubby all by myself after giving me a single demo how to feed her with the g-tube, I was left alone overnight in a small, dim, windowless room. I didn’t much sleep then any more than I had already, but I had more freedom to hold her close when I was tired so I could keep track of her easier.
It went well. My husband and I were informed we could take her home, so he brought the car seat. She cried badly the whole way. Upon getting home and inspecting the seat, it turned out she was just super uncomfortable because she didn’t fit it right due to having outgrown the infant insert. Which was a surprising realization, that she’d been in NICU long enough to do that. And being discharged to go home was like our adventure as new parents was finally starting, so we hadn’t considered checking that piece of car seat equipment.

Once out of her seat, I curled up with her in our large recliner we’d gotten with tax funds the year before so I had a seat comfortable enough to sit in while pregnant. She came home in her NICU Xmas outfit. But the house was quiet. And she was home.

Finally. I learned for myself how she had never been really satisfied with her breast milk volume, until I chanced increasing it. I was afraid she would vomit and aspirate to death, but the only thing that happened was she relaxed for the second time I’d ever seen. Like the first time she ever relaxed when I nursed her in the hospital right after I was told she was incapable.
She’s always, always shown me her strength. She is stubborn and fierce and frustrated and, when she smiles, filled with tranquility.
DAY 4: These Are A Few Of My Favorite Things
A few of my favorite things… Everything doctors said she’d never do.







DAY 5: Is she happy?

Far happier than if I hadn’t “wasted” my energy like her first NICU Attending, first Genetic Counselor and two shadows, and first GI Surgeon said.
She’s happier than when everything began. Her health has made huge strides because I didn’t give up, and I wasn’t afraid to try new approaches.
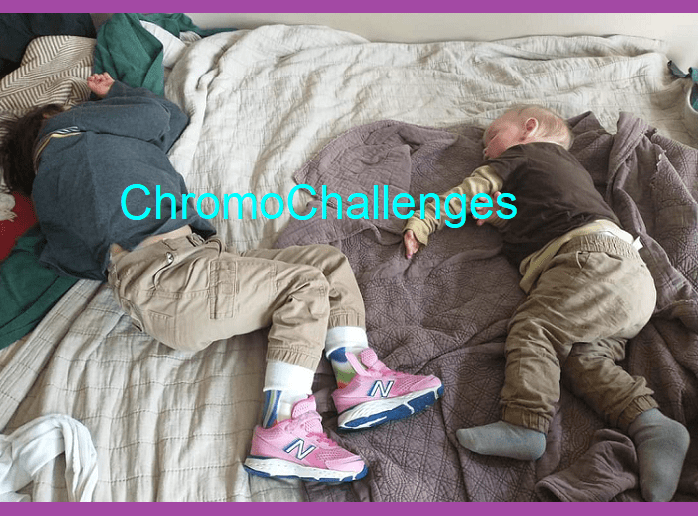
She’s happier since having a younger sibling, the first peer she’s had who doesn’t judge her or leave her behind.
Reading with her makes her happy.
Her and her brother’s show makes her smile.
Hugs make her giggle.
All sorts a Daddy’s Girl, him home from work makes her super happy too.
Being outside makes her happy, playing in the grass like her brothers do.
Enjoying tasty food and treats makes her happy.
She’s definitely happy doing just as much living as other children.

DAY 6: Trisomy Friends

Mostly I keep quiet because I don’t want to upset other, new, Trisomy families with my daughter’s progress. I remember when I also privately lamented (though also cheered!) the children who grew, while her doctors were so dour. I’m less reluctant to share her successes now, but I still try to stay somewhat sparing. Long-term, I don’t want her to feel like she’s performing. Though I do love to brag about my girl.
I have some Trisomy friends, all online, but wish she had closer relationships with some of her own like I’ve seen others be able to do. But as much as I want and need to socialize, not quite making it into the area after relocating in my third trimester of pregnancy put one kibosh on things, and quarantine kiboshed things some more.
So my girl primarily has her little brother to lean on. Who she’s taught bad habits like chewing paper. Awesome and mischievous duo.
DAY 7: A Day In The Life
Much of our days depend on whether or what appointments are upcoming. Since cracking a lot of her gut health needs, yearly hospital admittances dropped from 3-4 average to 1-0.
This past year, her schedule each day has largely consisted of me chasing the school’s online class schedule. But I’m now turning in paperwork to do homeschool starting this Fall. She hasn’t had adequate access to therapy resources, so I’m finally cutting our losses and setting them up as I want to see them be.
On low key days, she’s usually rough-and-tumble with her brother Eo. We do breakfast, lunch, and dinner syringe feeds with waters in the middles. We watch Cocomelon. I tend my kids.
DAY 8: Therapies & Medical Equipment

Moving from the Infinity g-tube motor and its incessant high-pitched beeps to quiet and greatly more portable syringe feeds changed the game quite a bit.
Hacking her health using functional health, biomedical approaches, and pattern tracking has led to progress far in excess of what her doctors dreamed. She tends to look one way on paper, but “independent” in person (because she can cruise, which is why we were refused home nursing services after moving).
Equipment currently using, or has used:
- A Stander.
- HyperVibe.
- Occasionally an Adaptive Stroller.
- Wheelchair for school bus transportation purposes.
- AFO footwear for better balance.
- “Airwalker” swing for calm and sensory processing.
- Walker.
- High-low chair.
- G-tube, which we make customized blends at home.
Therapies we’re doing, or have done:
- Rhythmic Movements for sensory processing.
- Yoga Ball for core strength.
- Swim Therapy.
- Stretches for better joint rotation.
- Wide-seat baby carrier to help seat hip joint properly.
- Soft splints for her wrists, but she learned to escape them.
DAY 9: Balancing Joy And Fear

I began the balance with denial of how I was being treated during pregnancy when ultrasound became questionable for some soft markers. Then I was angry because my wishes were ignored.
Then I was angry because any positive feelings I tried to express were rejected and stomped so I could “face reality”.
Then I was deeply, deeply depressed. Had she died at birth, I was resigned to join her. Then it became about showing medical how very, very wrong they were when she kept doing better than they said.
Aubby’s progress fueled my fire. I began to seek to support her thriving so we could give medical double flying birds together. I moved from potentially suicidal to something like pissed.
I began to research. I learned how to do better, and better than that, and better than that again. I had to. And it was fierce, exhausted joy. She won again, and again.

I have developed less fear as time goes on. I know how to choose my own way. I know how to find out how.
Recently, I began to really choose Joy Itself. To embrace what Is and make of That Stuff what I Will. I can choose Joy. I’m still working on allowing myself to live it too.
DAY 10: Siblings

Being my first full pregnancy, and a complicated situation, I wasn’t sure she’d have a sibling. After using Rebecca Fett’s book “It Starts With The Egg”, a solid vitamin regimen led to my second full pregnancy.
My kids are each other’s friend. I hope it stays that way. It’s not right of me to demand my second be responsible for Aubby when she’s older, but I do hope Eo takes initiative for her. Knowing just what to do for her is a lonely role. Lonelier still, I think, would be how lost she’d be without him if he didn’t, because nobody who hasn’t known her the way I do, and her father does, and her brother will… as they age will care for her the way she needs most. Family. Support. Genuine love that grows up knowing it without having to learn to accept.
Her younger brother is my gift to her, a friend for life. And maybe even a protector, for she will need it so much. But I also hope to continue hacking her health… maybe I’ll win that too.
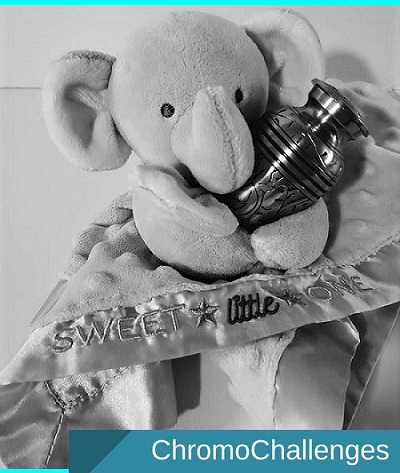
DAY 11: Grieving Normalcy
My grief for “normal” can be summed up the day I accepted that her equipment wasn’t meant to define her, but were tools. That’s as far as grieving normalcy went.
DAY 12: Inclusion, Disability, & Typical Kids
She hasn’t had much chance to mingle yet. When she did, she turned out to be the most mobile in her class. Then the 2020 Pandemic hit and nobody mingled at all.
When we’ve been at the park, she gets left behind because she’s not fast enough to keep up. She’s odd out because she’s tall, and her age, but her cognitive level and delays put her behind what’s expected. But then again, she often proves she understands far more than she can express.
Doctors often misjudge her; she looks one way on paper, but she blows it all away in person. She is my baby zebra.
Again, her sibling is her friend. He helps her, he doesn’t leave her behind. But with moving to do Homeschool, I hope to create a larger social opportunity for her.
DAY 13: Let’s Talk About PTSD
Part of me wants to ask: can we not? Before a fellow T18 mom’s post mentioned pushback from others being the worst of the experience, I had felt my hypervigilance was just… kinda my fault. That my trauma was something set into my skin and bones like the book “The Body Keeps The Score” (by Bessel van der Kolk, MD) digs into.
But what if trauma is less about the experience but the quality of care that comes in between and after? Acknowledgement that hurtful behavior happened? Some kind of apology?
As opposed to repeated lack of compassion, like a doctor with dark forecasts on multiple ultrasound visits, who doesn’t bother to balance the information with anything useful? Or how NICU staff may corner new parents who now have a medically fragile child and tell them over and over that they should prepare to lose them, imminently?
Parents of children who have precarious health isn’t automatic trauma. Any one event is unlikely to do it either, unless very sudden. But gather and gather, one after another, time after time, hurtful things… and then insist that despair is what’s appropriate. It’s an emotional abuse, if I’m any judge, and I must believe that the medical system isn’t even aware of the damage it inflicts because “ethics” have been decided and their “policies” tell them they’ve done their job right.
Somehow, what I’ve described is “right” for such situations.
But I, like some, saw alternative ways to bring hope to the situation. I saw differently, and hoped. What’s dire didn’t quite ruin my outlook, and I found answers in what was unsaid instead. I chased those answers.
What I’d call the nature of PTSD is inability to part with a need to relive pain. The pain must be relived until there’s closure. Otherwise, hanging on to pain because that’s all that’s left of what was loved IS the “closure”.
Time does help. But time may not be available if the pain is too much. Preventing this state is dependent on how those present treat the situation. Even darkness can be treated gently, and leave hope intact. Breaking a person’s spirit — when it might well happen anyway without such input — isn’t required.
DAY 14: Advice To New Parents
My thought on new parenthood: Don’t be afraid to cut your losses. Can’t? Oh well. Don’t want to? Don’t. Would rather do something your way? Do that then. Don’t fall for the Joneses and the judgment traps.
Also, advice on breastfeeding: My best help for breastfeeding equipment, if you plan to, forget electric pumps. Haakaa milk catcher/pump plus Lansinoh hand pump did FAR, far better by me than anything I ever tried, I was able to collect an extra 300 oz that way above the 1200 oz I stashed from when I had my first, and didn’t lead to non-response like I got to after my second and the Ameda didn’t do it for me. On demand and skin-to-skin for best results. Lean in to it early for the first months to establish supply, and then worry about tapering as needed. Best diet was chicken/protein, and loads of greens and fruit. Best latch: Hamburger breast to fit, flip chin down to correct latch. If painful, get the lip or tongue tie snipped ASAP. If supplement is desired, goat’s rue worked best with least affect on baby’s tummy through milk. Exclusively breastfed both my kids over a year.
On medical equipment: Trachs, high-low chairs, wheelchairs, AFOs, feeding tubes, and so on… They aren’t weaknesses. There’s no reason for shame or embarrassment. They are tools. Tools. Like eyeglasses others wear to see, or forks people use to eat, or properly fitting footwear.
DAY 15: How Can People Support You?
Don’t wait until my nerves are shot before wanting to offer to sit with me so I can put some energy towards anything else that needs doing. Most days, most all of my energy goes to my kid.
Parents often joke that their kids “suck the life out of them”. But then there’s some special needs parents, like myself, who must begin an Odyssey dedicated towards saving their child’s health.
We forget to eat. Eating’s a waste of time, or it might be that our grocery bill goes to specialized items due to food intolerances affecting our kid’s gut health.
We don’t sleep. Why sleep when we could be doing research with those “extra” hours? How can there be peace to sleep when we’ve been told, for certain, that our babies will die at any time before their time? We can’t allow that moment to be missed, it’d become our fault for letting them slip away in the night, alone, without our arms to cradle them so we can at minimum bid them bittersweet adieu.
We don’t do downtime. What purpose is downtime when we are required to know The Answer at all times? Not only how many diapers but their quality and trend. Not only how many times they ate in a day but the exact mL amount. Not just whats, but in-depth detail a sleuth would envy. Which then get brushed off as pat-on-the-head “mother’s intuition” rather than critical observations of minute health clues that managing medical practitioners could use to figure things out at the root…
That’s what gets trained into us during and in the days coming out of NICU. Doctors largely don’t advocate for babies like ours. Not trisomy kids, oh no. So we dedicate ourselves to our own “lost cause”, and somehow find ground because our “intuitions” lead us higher…
This hypervigilant state is where medical parents end up keyed to. Some feel abandoned by family, who stop visiting because they’re afraid of the sadness. Some feel abandoned by friends who suddenly not only might have chosen “kid free” lives to lead, but are then entirely relieved not to tread into our lives anymore, where fear rules. That’s great you’re living your best life, but we miss you, all of you, who once were our peers, our social scene, our support system.
“I don’t know how you do it.” We don’t either. But we have.
“I could never do that.” If you were backed into a corner that you could see a possible chance out of, yes you would. You’d follow it just the same.
When I say that offering your presence and time so your medical parent friends can think and feel about anything else but a terminal situation… that will even in the most promising of cases end with a child’s death or eventual destruction because doctors don’t spend their time on “incompatible” cases…
that contribution is a gift. It shows you aren’t afraid to stand by us. It shows that you care, at all. It allows us space to feel less lonely. Because we aren’t being brave. We’re being scared and angry, and scared and angry becomes the fuel used to try so hard to turn impossible tides.
DAY 16: Facing Our Biggest Challenges
One of my big challenges that continues over the years is having to inform myself. It was four years before more “normal” special needs concerns started to take shape. Finally not having to be four or five steps ahead of options that might present themselves was foreign to me. I started to just need to read up on what’s going on, rather than understand what might happen inside-out and backwards just in case yet another deep issue might present itself. The difference between those states has been the gradual stabilization of Aubby’s health as I’ve figured out how to eliminate toxins and address deficiencies.
Trying to find my way off the ride of perpetual overwhelm has been difficult. De-escalating hypervigilance was an anxiety-riddled side quest that presented itself just when I thought I was done with being worried all the time. The worry turned from what I needed to do for my daughter’s health to help her survive… Into what I needed to do to bring myself back to earth. At some point, I went numb. I was emotionally numb. Like, a state of zoned out that I did not have interest in the world around me. My only interests were caring for Aubby’s needs, her new younger sibling, and the answers that wifi access on my phone could bring me. But when the emergencies finally stopped rolling in constantly, then I had to begin to find myself again.
I’ve been asked if my marriage was very strained throughout all this. Luckily, I know my marriage is one of the few that does cleave to itself. My husband and I rarely, rarely get to enjoy intimacy. The last time we were afforded more than two hours to ourselves was in 2015 before Aubby was born — before our very peace was ransacked when the Maternal Fetal Medicine specialist thought we were dealing with Cystic Fibrosis and the every-appointment-from-then-on doom sounds he made began. But I guess we were taught patience with each other long before our Trisomy 18 journey began, when I became a stepmom in what was a difficult situation that the years hadn’t yet resigned to being.
For before our daughter and son was my stepkid and that situation. When Aubby was born, she was too medically fragile to be left with a sitter, family members had gone scarce due to her needs, and I didn’t know we should’ve had state healthcare and home nursing access. (The delivering hospital never submitted the paperwork, which I didn’t find out until she was a year old). Because I didn’t have help, that meant that she and I both had to ride with my husband on custody trips. Terminal diagnosis, feeding tube needs every 2-3 hours, diaper changes, pumping as needed, the chance to aspirate and choke to death from reflux if we couldn’t pull over easily… I had to monitor all of that during those 8-12 hour drives across state lines in all manner of weather. For a new baby with very big needs. We’re still a one-vehicle family, but quick hospital access at that time was required.
(So, if anyone on the other end of a custody setup has the ability to meet a medical parent AT MINIMUM HALFWAY, please, for the love of all that is good, PLEASE DO SO. Your cooperation affects safety and access to resources in an emergency. I know it’s “not fair”, but it’s a super easy way to “one-up” your ex, if that’s important to you, and be the better person.)
I guess the last really big thing I would call a “challenge” is when medical records must be transferred due to relocation. At the start of my third trimester with Eo, our family had to relocate from Missouri to Tennessee when my husband got work elsewhere. We moved in March 2019. At the time I originally wrote this post in March 2021, we were only just putting the finally appointments in place. So, it took two years (though, yes, there was a year of pandemic stalling it) to straighten out needs for medical specialists. Having to do that is a huuuuge headache for two reasons: Reason 1, not being able to keep a complete hardcopy of her medical records on hand is impossible due to hospital pushback on records, clinical notes omitted, or doctors refusing to be transparent. Missouri was more transparent (staff more friendly), Tennessee has really really not been so (but better tech and testing).
Reason 2, Trisomy 18 kids are zebras and new specialists freak out when they see the medical file. It is super important to be sure all participating medical staff have a copy of Baty’s study (Part 1 linked below) of the “natural history of Trisomy 18” for their records so Trisomy parents aren’t blamed for lack of developmental expectations. Particularly, the following three articles:
DAY 17: What Is Your Hope For Our Babies?
I hope…
That my journey shows others that there are better ways to be, and how little things make the biggest impacts. That new trisomy parents understand that unleashing backbone is the key to advocating strongly.
That more families in the trisomy community come forward so that our stories are shared to change how our kids are treated… so that they are treated. That doctors stop edging out our kids to pulmonary hypertension and other unrecoverable states so they can get prompt heart intervention and can grow.
That other families who have developmentally typical children can look on our babies with inclusiveness and compassion. For more people to see and acknowledge the value all people born to this world have in existing… including our Trisomy Warriors who arrive Earthside already fighting to show how actually compatible with life they are.
DAY 18: How Has Your Child Changed Your Life?
Had I never had kids — as I was almost 30 and had 3 miscarriages under my belt by then while certain family members were busy asking when I was going to do the family thing for real — I was on the edge of preparing to redefine my life a different way and just focus on career and personal leisure with my partner.
One of the greatest lessons I feel I’ve learned is how grief and love and beauty intersect. That was something that came to me in the quiet moments between crises in the NICU. And later after she was discharged home and I hung my attention on every breath she took. Since 2018, I have been a stay-at-home mom due to unreliable home nursing care. But that was also the year I started this website, and doing this on purpose.
In my teenage years, thinking about my “Someday”, I always imagined just one child. A girl with the power to overcome. I was gifted that exactly. And then my teenage self used to think, “But IF I wanted, then a second too. A younger sibling, a brother like I had growing up. But not by accident, I want to know I wanted my kids, and for them to know I wanted them.” And you know what? I achieved my son, too, exactly, after I went out of my way to follow that vitamin regimen. What I didn’t anticipate was why I’d have to struggle, or the hurdles that came. But I also didn’t know I’d learn so much, or see how expanded my capacity for feeling would be, or that I’d grow a stronger backbone for them.
My husband has also mentioned to me how Aubby’s changed his life. He wouldn’t have known to become the physical therapist assistant that he did. And that path led to his hiring into a career he loves, doing work he loves, and starting his online pain management work that he also loves. I’m incredibly excited for him and his growth.
I still have a picture in my heart of what I want my life to be. I have projects at hand leading me forward. Though surrendering, also, to what my life wants me to be is another thing, side adventures. Feeling gratitude for whatever life is at any one moment is good too. There’s a lot of beautiful the more I’ve purposely let it in and sought it out.